State-of-the-art technology allows us to provide comprehensive treatment options for patients close to home. This video shows what our radiation treatment rooms and two advanced TrueBeam™ linear accelerators look like to help you know what to expect your first radiation therapy appointment.
Targeted cancer treatment
If you have been diagnosed with cancer, your doctor may recommend you have radiation therapy. Radiation therapy uses high energy x-rays to destroy cancer cells and shrink tumors. About half of all cancer patients receive radiation therapy as part of their cancer treatment.
Radiation therapy can be used alone or with other types of cancer treatments such as chemotherapy or surgery. Some patients receive more than one type of radiation therapy.
The goal of radiation therapy is to destroy as many cancer cells as possible, while limiting harm to healthy cells and tissue. Some types of radiation are targeted to treat only a very small area of your body, while other types are used to target large areas. Before you begin treatment, your doctor will determine the right type of radiation therapy for you.
Our team uses the latest advances in radiation therapy to treat all types of cancer. We have been accredited by the American College of Radiation Oncology for quality patient care including the safe and effective use of radiation therapy.
Learn how radiation therapy could help you. Contact us today.
The Aalfs Family Foundation
Radiation Oncology Department
How radiation therapy works
Cancer cells grow faster than normal cells in the body. Radiation therapy targets rapidly growing cancer cells by damaging the DNA or genetic material in the cells that controls cell growth. While most normal cells can recover from the effects of radiation, cancer cells can’t repair themselves easily and are destroyed through radiation.
There are two types of radiation therapy: external radiation and internal radiation. Patients can receive one or the other, or a combination of the two.
EXTERNAL RADIATION: This is the most common type of radiation and uses a machine outside your body to aim radiation at a targeted area. External radiation is given on an outpatient basis and is painless – similar to having an x-ray taken. It can be used to treat most types of cancer including cancer of the bladder, head and neck, pancreas, brain, breast, cervix, larynx, lung, prostate, and vagina. External radiation can also be used to ease pain when cancer spreads to other parts of the body, for example into the bones.
INTERNAL RADIATION: This type of radiation is placed inside your body in or near the targeted cancer cells. It is put in the body by swallowing radioactive material, through an injection in the skin, or by being surgically implanted. The radioactive material can be left in place for a few hours or even days. As time passes, most of the radiation will go away, even though the implant stays in your body.
Your doctor will determine the right type of radiation for you based on your diagnosis, the location of your cancer, your general health, and your medical history.
Types of cancer treated with radiation therapy
Radiation therapy is used to treat many types of cancer including:
Prostate
Skin
Soft tissue sarcomas
Spine
Stomach
Uterus
Brain
Breast
Cervix
Larynx/other head and neck cancers
Lung
Pancreas
It is also used to treat blood and lymphatic system cancers including leukemia and lymphoma. In other cases, radiation therapy is used in areas that do not show any evidence of cancer. This is called prophylactic radiation therapy.
Palliative radiation therapy is another type of radiation therapy that is sometimes used to reduce pain from cancer that has spread to the bones or other parts of the body.
Radiation can also be used to prevent bone growth after joint replacement surgery when needed. Called heterotropic therapy, the radiation oncologist collaborates with your orthopedic surgeon post-surgery for the single treatment.
Treatment planning before radiation therapy
Before you receive radiation therapy, your coordinated care team will review your case to determine the amount and type of radiation that is right for you. This is an important step in your treatment planning process.
Your radiation therapy team includes:
Radiation oncologist, a doctor who specializes in treating cancer with radiation
Dosimetrist who determines how to deliver the prescribed radiation dose to the targeted area while limiting the dose to the surrounding healthy tissue
Radiation physicist who calibrates the equipment and makes sure the radiation treatment machine delivers the correct amount of radiation to the right area
Radiation therapists who deliver the radiation treatment
Nurses who perform routine patient evaluations during radiation treatment and monitor side effects.
If you need external radiation, your radiation oncologist will use a process called simulation to determine where to aim the radiation in your body. During simulation, you will lie very still on an examining table while a radiation therapist uses a CT scan or PET scan to determine the exact place on your body where radiation will be aimed.
These images are transferred to the dosimetrist’s planning system. The planning process can take several hours, and in most cases you will not receive treatment on the same day as the simulation.
Areas of your body that are targeted for radiation will be marked with either a temporary mark or possibly a small permanent tattoo to show where the radiation should be aimed.
Depending on the type of radiation treatment, your radiation therapist may make body molds to keep you from moving during treatment. The molds are usually made from foam or plastic. Shields may also be made to protect organs and tissues near the treatment site.
What to expect during radiation therapy
During radiation therapy, you will lie down on a movable treatment table. A linear accelerator – or machine that generates energy or radiation – will deliver beams of radiation to your tumor from multiple directions or angles.
Depending on the amount of radiation, the linear accelerator can be used to destroy cancer cells on the surface of the body or deeper into tissues and organs. The strength of the radiation will be customized based on your unique treatment needs.
Patient safety is a top priority, and several safety measures are built into the linear accelerator so that it only delivers the prescribed dose for your specific treatment plan. During treatment, your radiation therapists will continually monitor you.
Some patients are concerned that radiation therapy will make them radioactive after treatment. External radiation therapy does not make patients radioactive, and patients do not need to avoid being around other people because of their treatment.
Internal radiation therapy that involves sealed implants can make the area around the implant radioactive. Because of this, some patients need to stay in the hospital during internal radiation treatments as well as avoid close contact with children and pregnant women for a set time period.
Radiation therapy can cause some side effects. The type of symptoms can vary depending on the areas targeted during radiation therapy. The most common side effects include:
Diarrhea
Fatigue
Hair loss
Nausea and vomiting
Sexual problems
Skin changes
Throat changes
The radiation oncology nurses can help answer questions related to your specific treatment plan and possible side effects. They can be contacted at (712) 252-9456. If you have questions regarding an upcoming radiation treatment appointment, please reach out to our qualified radiation therapists at (712) 252-9380.
Types of radiation therapy treatments
Linear Accelerator (LINAC)
Our two TrueBeam™ linear accelerators are state-of-the-art machines that can perform highly complex Intensity Modulated Radiation Therapy (IMRT) and Image Guided Radiation Therapy (IGRT) treatments. The machines work with computer technology to assist in targeted and advanced forms of radiation therapy.
Image Guided Radiation Therapy (IGRT)
IGRT is the use of treatment room imaging modalities (i.e. x-ray and CT scans) to precisely target a tumor for daily radiation treatment. Using image guidance for tumors affected by organ motion and day-to-day set up changes can lead to increased tumor response and/or decreased side effects from treatment. Utilizing cone-beam CT images allows overlaying of the daily CT scan upon the planning scan assuring precise setup and treatment.
Intensity Modulated Radiation Therapy (IMRT)
IMRT is another treatment technique used to deliver highly accurate doses of radiation to irregularly shaped tumors with fewer adverse side effects. Pencil-thin beams of varied intensity conforms the radiation to the shape of the tumor, allowing physicians to attack the cancer with the higher doses of radiation while minimizing damage to nearby healthy tissue and organs.
Volumetric Modulated Arc Therapy (VMAT), a type of IMRT, moves around the patient while ever-changing the shape of the beam as it delivers the radiation dose.
Because IMRT equipment is highly specialized, not every cancer treatment center offers IMRT. June E. Nylen Cancer Center has a strong and ongoing commitment to bringing our patients the best and most current therapies.
Stereotactic Radiosurgery (SRS)
Stereotactic Radiosurgery (SRS) allows tumors to be destroyed non-invasively, also known as “surgery without a scalpel.”
Radiosurgery is a radiation delivery procedure that precisely delivers large radiation doses to tumors and other relevant anatomical targets in a single session. The goal of this non-invasive procedure is to destroy, or render inactive, the target anatomy without harming healthy tissue and without involving traditional surgery and avoiding anesthesia.
Download our Patient’s Guide to SRS Brochure
Stereotactic Radiation Therapy (SRT)
Stereotactic Radiation Therapy (SRT) is similar to SRS but instead of being completed in one single dose, the radiation is delivered over a course of several sessions (typically up to five).
SRT is also known as fractionated radiosurgery, because a fraction of the total radiation dose is delivered at each session. SRT is used to treat tumors or abnormalities in the brain, head, neck, and spine. It may also be used to treat tumors or abnormalities in other parts of the body—in the lungs, liver, kidneys, and pancreas, for example.
Stereotactic Body RadioSurgery (SBRT)
Stereotactic Body Radiotherapy, or SBRT, a type of external radiation therapy, is available at the Nylen Cancer Center. It is most commonly used when a tumor is found very early. SBRT allows us to be able to treat small tumors very precisely by limiting patient movement with various technologies. This spares surrounding normal tissue.
Internal Radiation Therapy – Brachytherapy
Brachytherapy is a form of radiation that involves the placement of radioactive sources into a tumor or in an area where a tumor was removed. This technique allows for the delivery of high doses of radiation therapy while simultaneously sparing normal tissue.
The word “brachytherapy” means “short therapy,” appropriately implying that the radiation is limited to short distances. This results in decreased toxicity to normal tissues and also allows a higher radiation dose to the tumor.
Internal radiation therapy (or brachytherapy) uses high doses of radiation that is placed very close to or inside the tumor.
The radiation source is usually sealed in a small holder called an implant. Implants may be in the form of thin wires, plastic tubes called catheters, ribbons, capsules, or seeds.
The implant is put directly into the body. Internal radiation therapy may require a brief hospital stay. The radiation is emitted outward, unlike external beam radiotherapy, where radiation travels through normal tissue in order to reach the tumor.
Brachytherapy is often used to treat prostate and gynecologic malignancies. The radiation oncologist travels to the Siouxland Urology office to perform this procedure for prostate cancer patients, increasing patient convenience.
3-D Radiation Therapy
The June E. Nylen Cancer Center offers the innovation of 3-Dimensional Conformal Radiation Therapy. Traditionally, the planning of radiation treatments has been done in two dimensions (width and height). Three-dimensional conformal radiation therapy (3-D Therapy) uses computer technology to allow doctors to more precisely target a tumor with radiation beams by using width, height, and depth.
A 3-D image of a tumor is obtained using a CT scan, MRI, or PET scan. Using information from the image, special computer programs design radiation beams that “conform” to the shape of the tumor.
Because the healthy tissue surrounding the tumor is largely spared by this technique, higher doses of radiation can be used to treat the cancer without increased side effects. Improved outcomes with 3-D therapy have been reported for nasopharyngeal, prostate, lung, liver, and brain cancers.
Utilizing innovative technology to increase treatment accuracy and patient comfort during radiation therapy
Donor support for radiation therapy
At the June E. Nylen Cancer Center and the Aalfs Family Foundation Radiation Oncology Department, we take extra precautions to make sure that every patient receives minimal radiation exposure during treatment. We use AlignRT®, the premier radiation therapy guidance system, for Surface Guided Radiation Therapy (SGRT) with two state-of-the-art TrueBeam™ linear accelerator treatment machines. This system, from Vision RT, has been shown to reduce radiation exposure to healthy tissue.
AlignRT tracks your body surface in real-time, detects any motion as you hold your breath with sub-millimeter accuracy, and pinpoints your radiation treatment to the specific cancer area, dramatically lessening unwanted radiation exposure to any healthy tissue and reducing the risk of side effects. While used head-to-toe and for all radiation treatment, a valuable example of the benefit of AlignRT to ensure optimal patient positioning and radiation accuracy is protecting your heart while you’re treated for left-breast cancer.
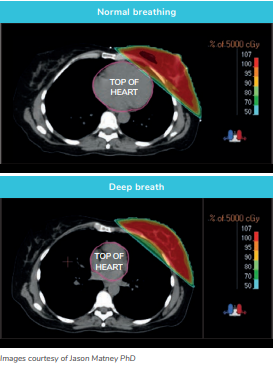
When treating left-breast cancer AlignRT can help us make sure your heart is in the right place. For some patients, we utilize a technique called Deep Inspiration Breath Hold (DIBH) to move the heart away from the breast during therapy. This is challenging because patients breathe in different ways at various times, and may move their body like arching their back during a deep breath in. AlignRT uses a 3D camera system to help position you accurately before radiation therapy and then to track your body surface in real-time through the DIBH, ensuring you keep in the proper position during treatment. Using your external skin surface, the technology monitors your movement and knows exactly where you are at any moment to within a fraction of a millimeter.
Another benefit of the AlignRT guidance system being used during radiation therapy at the June E. Nylen Cancer Center is that it can eliminate the need for tattoos and skin marks for many patients. The technology projects a random series of patterns on your skin, acting like thousands of virtual tattoos. These images are input into a software program that monitors your positioning with sub-millimeter accuracy and ensures you are treated in the correct position. AlignRT has been shown in several studies to be at least as accurate as either marks or tattoos for positioning patients before treatment therapy. Many patients are happy and relieved to not have a permanent reminder of their diagnosis and treatment. Not all radiation treatment centers can offer tattoo/mark-free radiation.
For more information about the AlignRT radiation therapy guidance system, talk to our Radiation Oncology team or click here.
The June E. Nylen Cancer Center launched a capital campaign in the Fall of 2017 to raise funds to purchase their second new TrueBeam™ linear accelerator radiation treatment machine. We are extremely grateful for so many donors who believe our community deserves to have the best technology for cancer treatment close to home.
Thank you to these naming donors of our Hope and Healing Campaign:
Radiation Oncology Department - Aalfs Family Foundation
Radiation Treatment Room 1 - Hepar BioScience, LLC
Radiation Treatment Room 2 - Commercial Chaos for a Cure
Radiation Exam Rooms:
Central Bank
Vibeke T. Jensen in memory of Aasa T. and Svend A. Jensen
State Steel and Sioux City Compressed Steel
U.S. Bank
Radiation Nurses Station & Waiting Room - empirical
Diagnostic Imaging Suite - Klinger Companies, Inc. and Gleeson Family Foundation
Patient Navigation Wing - Chesterman Family Foundation
Laboratory Department - Ted De Vries in Memory of Jo De Vries
Medically Integrated Dispensary - Jeannine Anderson in memory of W.E. Woodall